Keratoconus
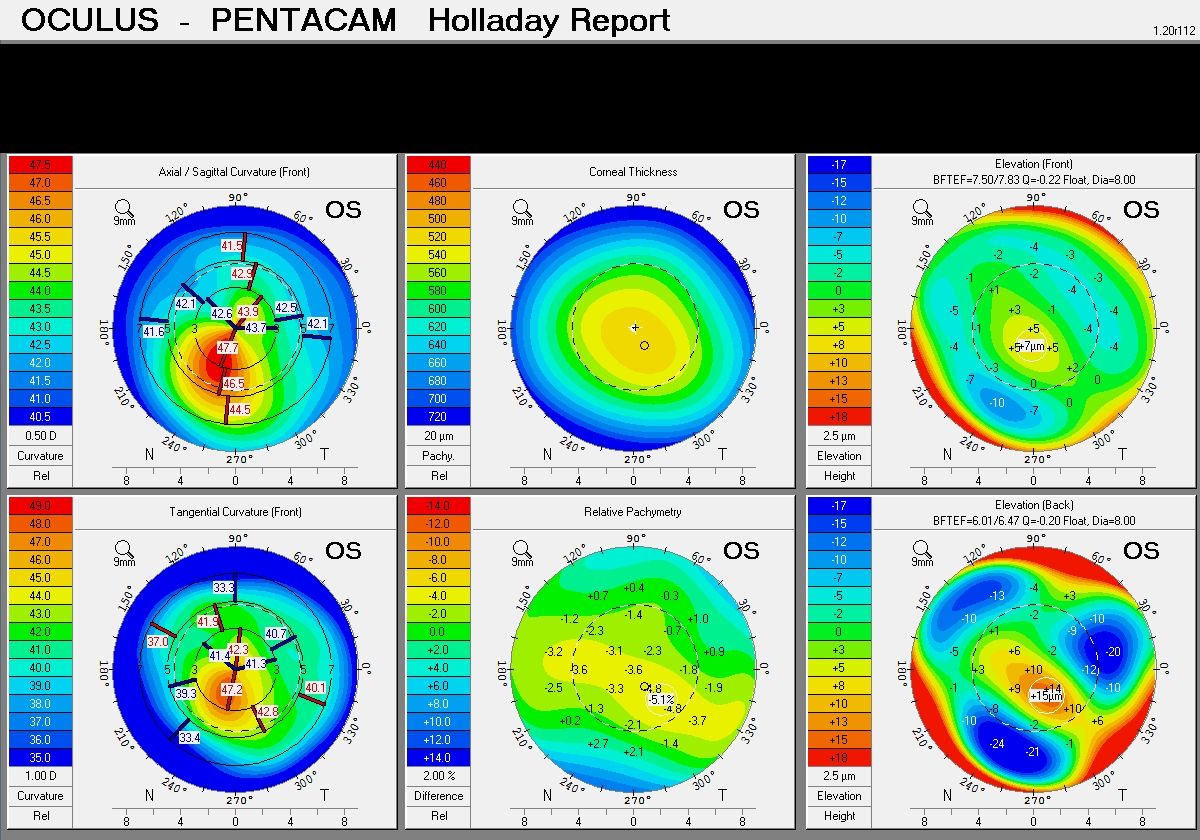
Keratoconus is a common condition affecting the strength of the cornea. The cornea is the glassy window at the front of our eyes (where you would poke yourself if you stuck your finger in your eye!) Keratoconus is largely related to inherited genetic factors. Most people do not have an affected relative, but if it is in your family you are significantly more likely to develop keratoconus. The incidence of keratoconus is about 1 in every 500 people, and about 10 times higher in people with an effected close relative. People with keratoconus develop progressive thinning and steepening of their central cornea. This results in shortsightedness and astigmatism (which means the cornea looks like a rugby ball instead of a soccer ball). Early cases can only be diagnosed with corneal mapping, called corneal topography. As the weakening progresses the rugby ball shape becomes more and more distorted, which is irregular astigmatism. Keratoconus usually progresses from mid teens until mid to late 20s, but may stabilise younger than this. It is often very asymmetric, with 1 eye more badly affected than the other. Some people may not notice they have a problem until 1 eye is quite advanced. It is made worse by eye rubbing, so is more common and more severe in people with itchy eyes such as allergies and hayfever. It is also more common in some medical conditions, such as Down syndrome, atopic dermatitis and Ehlers-Danlos syndrome. People with itchy eyes and keratoconus are strongly advised to minimise (preferably stop) eye rubbing. Use of over the counter antihistamine eye drops such as Zaditen or Patanol may be vey helpful for this.
Treatment
Glasses
Keratoconus may be well corrected by simple glasses. Glasses can correct regular errors such as shortsightedness and astigmatism. They cannot correct the irregular astigmatism which is a common feature of more advanced keratoconus, so many people with significant keratoconus will not achieve adequate vision with glasses. People with very mild keratoconus may even have normal vision without any correction at all.
Contact lenses
Modern contact lens designs and materials mean that many people with moderate keratoconus will achieve excellent comfortable vision with contact lenses. More mild cases may do well with soft lenses, but most people will get better vision with a hard lens. These compensate for the irregularity and usually give very good vision, but are more difficult to fit optimally. Most optometrists are skilled at fitting and prescribing normal soft contact lenses, but if you require a specialist hard lens you may be referred to an optometrist specialising in contact lens fitting.
Cross-linking (CXL)
CXL is a new treatment which is extremely effective at halting further progression of keratoconus. It was developed in Germany in 2003 and has been shown in many studies worldwide to be very safe and highly effective. In some cases there may be some measurable improvement in vision, but this is unpredictable and usually quite mild. CXL involves application of vitamin B12 (riboflavin) eye drops and then exposure to low dose ultraviolet light. This creates a chemical reaction which results in a controlled scar forming in the cornea. This remains clear but is much tougher than the weak keratoconic cornea and is resistant to further stretching and thinning, halting progression in most cases.
CXL has been shown to be successful at stopping progression in 96-98% of cases. Between 1 and 2% of cases may lose a moderate amount of vision afterwards – like any surgical intervention there is a small risk of complications. Because there is not usually a large improvement in vision it is best done for people who are still in the early stages of keratoconus. Many people with keratoconus will already be stable and will never get worse, especially those over 30 years of age. There is no point doing a stabilising treatment for someone who is already stable. Because of this and the low risk of visually significant complications it is preferred to be sure that the keratoconus is actually progressing before going ahead with CXL. This is best done with corneal mapping done on 2 separate occasions, usually 3 to 6 months apart. Well documented deterioration of glasses prescription in a young person may be a reasonable alternative confirmation of progression.
After the procedure there is usually significant discomfort or pain for 2 days, blurry vision for 2 weeks and sensitivity to light for up to 2 months. Most people will take a week or so off work or study. Slow improvement in the amount of keratoconus may occur for up to 2 years after treatment. Most people can resume use of their old contact lenses within 2 weeks. Treatment of both eyes on the same day is almost always a bad idea because of the post-procedure discomfort, poor vision and risk of loss of vision in both eyes. Treatment of stable eyes which are not progressing “just in case” is also not recommended. However, if the keratoconus is progressing the earlier the treatment is done the better the final result, and complications are more common in very thin or very steep corneas. Advanced corneal thinning means cross-linking should not be done as the treatment will go right through the cornea and damage the inside of the eye.
ICRS are reinforcing implants placed in the cornea to improve vision in people with keratoconus. A circular tunnel is created in the cornea by a femtosecond laser and the segments threaded into the tunnel. The whole procedure takes about 10 minutes and is usually painless. The advantages of ICRS include the usually very quick recovery (a day or 2 is usual), the painless nature of the procedure and the fact that it is reversible. If there are significant problems the segments can be easily removed and the cornea returns to its’ previous shape. The chances of scarring of the central cornea and loss of vision are therefore very low. The downsides to ICRS include that it takes up to 3 months for vision to stabilise afterwards and most people will notice halos at night around light sources. This is reflection of the light from the edge of the rings when the pupil is large at night, but most people with keratoconus have poor night vision before treatment anyway. The biggest problem with rings is the effect can be quite unpredictable. About 20% of people won’t notice much change in their vision, and many people still need contact lenses afterwards. Often though it is much easier to fit lenses afterwards, and many people can wear soft lenses instead of hards which may be more comfortable.
I find ICRS to be best suited for people with moderate keratoconus who are intolerant to their hard contact lenses. Some people will achieve very good unaided vision afterwards, especially if they were relatively mild to start with, but these results are difficult to predict. In some cases combining ICRS with CXL may give even better results, but with slower recovery and slightly higher risk of complications.
Corneal Transplant
Until fairly recently the only treatment for keratoconus was contact lenses or a corneal transplant. CXL and ICRS mean that fewer people now need transplant surgery, but for severe keratoconus it is still the best (and only) treatment. A corneal transplant (corneal graft means the same thing) involves cutting out the weak keratoconic part of the cornea and replacing it with a healthy strong cornea. This is from someone who has died and donated their eyes for surgery. In 2012 1000 corneal transplants were done in Australia, with keratoconus being the most common reason to have one. Keratoconus has the highest success rate for corneal transplants. 90% of people will get vision good enough to drive. The average graft survival time for keratoconus is 20 years. Corneal transplantation is a significant surgery, and there is a risk of complications. These include rejection of the transplant, infection, cataract, high astigmatism and graft rupture with trauma. In some cases it is possible to preserve the inner lining of the patient’s cornea, which is called a deep anterior lamellar keratoplasty (DALK) but in other cases a full thickness replacement is needed (penetrating keratoplasty or PK). A DALK has lower risk of rejection, but unless the remaining layer is extremely thin the resulting vision can be poor. The thinner the layer the better the vision but the higher the chance that it tears and a PK is needed.
Recovery from a corneal transplant is usually lengthy. Discomfort rather than pain is usual, though most people experience a scratchy sensation for the first few weeks. Most people take about 2 weeks off work, though obviously this depends on the type of work. Recovery of useful vision may be between a few weeks and 2 years. The sutures are not dissolvable and most need to remain in place until 12 months after surgery. Glasses may be possible after 3 months. Swimming is not recommended for 6 months and contact sports should be avoided permanently. Eye drops will often be required in low dose lifelong. For more information on post-operative care please see my corneal graft post-operative instructions.
Summary
Keratoconus is a common treatable eye condition. People who are not progressing and have good comfortable vision with contact lenses do not need any treatment, though regular monitoring for progression is recommended. Aggressive management of allergies and eye rubbing is critical. Early or moderate cases with definite progression will usually have cross-linking. Moderate cases which are contact lens intolerant may benefit from corneal rings. Advanced cases where no other treatment will work usually get good vision with a corneal transplant. Modern corneal mapping can detect very early cases, and with cross-linking being so effective and safe early detection is highly desirable. It is likely that with early detection, cross-linking and modern contact lenses more invasive surgical treatments will become less frequent.