Epiretinal Membrane
Also known as macular pucker, premacular fibrosis or cellophane maculopathy, an epiretinal membrane is a thin sheet of fibrous tissue that can grow over the surface of the retina. The retina is like the film in a camera. In some cases the epiretinal membrane remains mild and does not significantly alter the vision however when an epiretinal membrane grows it may damage the macula and cause the vision to become distorted and blurred. The macula is the most important part of the retina and gives us sharp central vision for reading. If the membrane continues to progress, permanent damage to the central vision may occur.
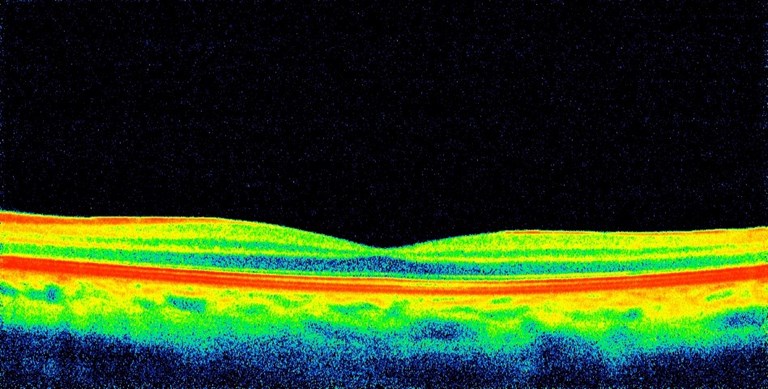
Fig 1. OCT scan of a normal retina
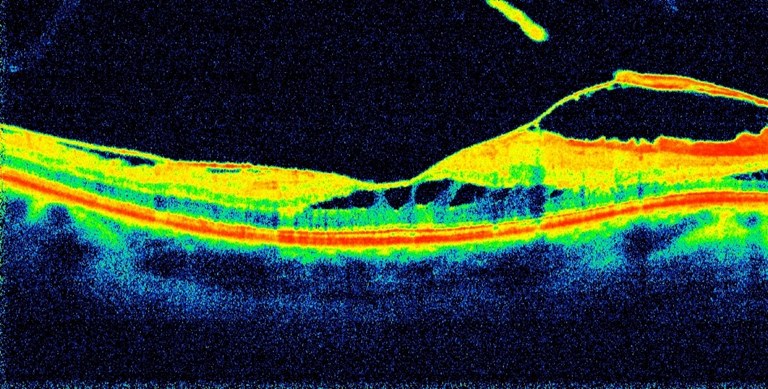
Fig 2. OCT view of an Epiretinal Membrane
What causes an Epiretinal Membrane?
In most cases an epiretinal membrane occurs as a result of age changes in the vitreous jelly which cause it to separate from the retina. These changes occur in everyone and are normal, but for unknown reasons, some people develop scarring or membrane formation. Occasionally an epiretinal membrane will develop in an eye as a result of retinal tears, detachment, trauma, inflammatory disease, blood vessel abnormalities, or other pathological conditions and it is important to see an experienced Vitreoretinal surgeon to evaluate for these.
What is the treatment for an Epiretinal Membrane?
If an epiretinal membrane is mild and not interfering with your vision, no treatment is required. An annual review and OCT scan to monitor for progression are important. Once a membrane develops, it will never go away on its own. Once the membrane begins to affect your vision, it can be removed surgically.
What is Epiretinal Membrane surgery like?
Modern surgery allows us to very successfully remove the epiretinal membrane. The surgical procedure is called a Vitrectomy. This is performed using very fine microsurgical “keyhole” instruments to gently peel the membrane from the retina. The surgery usually takes less than one hour, and is usually performed under “twilight” sedation using local anesthetic and is not painful. It is day surgery and you do not need to stay in hospital over night. As long as you do not have a retinal detachment you will NOT need to position face down after surgery.
What is the chance of my vision improving?
In 90% of cases, once the membrane is removed, the distortion and the vision should improve. How much vision is restored depends on your general health, the health of your eye and the length of time that the membrane has been present. In general, most people regain around 50 % of the vision they have lost, however some will gain more and some less. In general the milder the membrane and less time it has been growing, the better the prognosis. Your vision will continue to improve slowly for up to one year.
What happens after surgery?
Following surgery, the vision will be mildly blurred for the first week due to mild swelling. For the first 24 hours it is best to rest at home. Computer work and watching television are fine.
A protective shield is recommended for sleeping, for the first week after the surgery and you will be required to have eye drops for one month. You can resume light activities a few days after surgery. Depending on your type of work, some people return to work within a few days, others may require a week or longer off for heavy physical activity.
What are the risks of surgery?
- Although Epiretinal Membrane surgery is a very successful procedure, one should be aware that all surgery has risks, and occasionally problems can arise following surgery.
- A cataract may develop earlier than would be expected during the normal aging process.
- The eye may develop increased pressure (glaucoma) and medication may be required.
- Retinal tears or detachment of the retina may develop during surgery, or following surgery, and may require further surgery. correct these.
- Infection and haemorrhage are very rare risks which may occur with any surgery. If you notice pain or decreased vision following surgery, contact our consulting rooms or your surgeon’s mobile as soon as possible. Infections often treatable if detected early. A severe infection or severe bleeding however can result in permanent blindness, but this is very rare, much less than 0.1%.
Intraocular gas
- The chance of this being required is less than 1%. If you have a gas bubble it is very important not to sleep on your back, or lie on your back for extended periods, as in this position the gas bubble will rub on your lens
- While a bubble is present, you MUST NOT FLY in an airplane. This could result in blindness as the bubble expands with altitude.
- If you need to travel over the Toowoomba ranges please mention this to your doctor.
- If you require surgery of any other kind over the following two months you must tell the anesthetist about the gas bubble as nitrous gas anaesthetics will cause the bubble to expand and cause severe vision threatening pressure rises.